소아 천공충수염과 백혈구계산 및 적혈구침강속도 증가의 연관
High white blood cell count and erythrocyte sedimentation rate are associated with perforated appendicitis in children
Article information
Abstract
Purpose
To investigate the predictors of perforated appendicitis (PA) in pediatric patients with appendicitis seen in the emergency department.
Methods
We retrospectively reviewed 564 pediatric patients (< 16 years) who visited the emergency department and subsequently had pathologically confirmed appendicitis from 2005 through 2014. Clinical features, inflammatory markers, including the white blood cell (WBC), neutrophil, and lymphocyte counts, neutrophil-to-lymphocyte ratio, C-reactive protein (CRP) concentration, erythrocyte sedimentation rate (ESR), and the Alvarado score were compared between the patients with and without PA regarding their predictability of PA.
Results
Of 564 pediatric patients with appendicitis, 204 (36.2%) had PAs. The patients with PA had longer duration of symptoms and median length of hospital stay, more frequent nausea and vomiting, and higher median WBC and neutrophil counts, neutrophil-to-lymphocyte ratio, ESR, and CRP concentration. Overall, WBC count showed the highest sensitivity of 79.9% and negative predictive value of 82.6%, and CRP concentration had the highest area under the receiver operating characteristic curve of 0.72. Multivariable logistic analysis showed that WBC count > 13.5 × 109/L (odds ratio [OR], 3.27; confidence interval [CI], 1.49-7.18; P = 0.003) and ESR > 15 mm/h (OR, 3.18; 95% CI, 2.13-4.74; P < 0.001) are independent predictors of PA.
Conclusion
WBC count and ESR might be better predictors of PA in pediatric patients with appendicitis in the emergency department than the Alvarado score and CRP concentration.
Introduction
In pediatric patients, perforated appendicitis (PA) requires an expeditious diagnosis and proper surgical treatment [1]. PA is more common in patients aged younger than 4 years than in adolescents (< 70% vs. < 15%) [2-4]. The nonspecific symptoms and difficult communication with pediatric patients may delay the diagnosis [4,5]. This delay could complicate the surgery, increase the length of hospital stay, and aggravate the outcome [5-7]. The outcome might be improved with an early prediction of PA in the emergency department (ED).
The Alvarado score has been frequently used in predicting appendicitis in adult patients [8-9]. However, in pediatric patients, some components of this scoring system, including migration of pain, anorexia, and nausea, are inaccurate in predicting appnedicitis [8-10]. Given this poor predictability of appendicitis, the Alvarado score might also be inaccurate in predicting PA in pediatric patients. To compensate for this drawback, other potential predictors of PA, such as laboratory findings and imaging modalities, have been studied [4,11-15].
Inflammatory markers measured in the ED are readily and rapidly available for pediatric patients with suspected PA. A high C-reactive protein (CRP) concentration and white blood cell (WBC) count are associated with PA, while there are few studies on other inflammatory markers, such as erythrocyte sedimentation rate (ESR), and the Alvarado score in predicting PA in pediatric patients in the ED [11-16]. Therefore, we aimed to investigate the predictor of PA by comparing inflammatory markers, the Alvarado score, and other features related to PA in pediatric patients who visited the ED and subsequently had pathologically confirmed appendicitis.
Methods
We retrospectively reviewed pediatric patients aged younger than 16 years who visited the ED and subsequently had pathologically confirmed appendicitis between January 2005 and December 2014. After obtaining approval from the Institutional Review Board (IRB No. OC17RESI0044), we collected and analyzed the patient data. This hospital is a tertiary teaching hospital, and the ED treats approximately 50,000 patients annually. The 564 pediatric patients with appendicitis were identified based on pathologic reports and/or surgical notes. The patients classified into 2 groups depending on documentation of PA on pathologic reports: the perforation and non-perforation groups.
The clinical features were obtained from a chart review, including age, gender, body temperature, duration and migration of abdominal pain, anorexia, nausea, vomiting, right lower quadrant tenderness, and rebound tenderness. We recorded the laboratory findings obtained within 2 hours of presentation, including WBC count, neutrophil, and lymphocyte counts, neutrophil-to-lymphocyte ratio, red cell distribution width, serum CRP concentration, ESR, and glucose. To assess the outcomes, length of hospital stay was recorded. The Alvarado score [9] was retrospectively calculated in all patients. We classified the pediatric patients into 4 score groups. A score of 0 to 4 indicates non-appendicitis, 5 or 6 for possible appendicitis, 7 or 8 for probable appendicitis, and 9 or 10 for very probable appendicitis.
The statistical analyses were performed using SPSS ver. 12.0 (SPSS Inc., Chicago, IL). Clinical features of the 2 groups were compared using the Student t-tests or Mann-Whitney U-tests for continuous variables. The chi-square tests were used to assess categorical variables. The prediction of PA was analyzed using receiver operating characteristic curves and predictive values, including sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV). A cutoff value with 95% confidence interval (CI), which maximized area under the curve (AUC), was selected. Multivariable logistic regression analysis using the variables having P < 0.05 from the univariable analyses was used to identify independent predictors of PA. The results are presented as odds ratios (ORs) with 95% CIs. P < 0.05 was considered to be statistically significant.
Results
Clinical features of the study population
Of 564 pediatric patients with appendicitis, 322 (57.1%) were boys, and 204 (36.2%) had PA. Mean age of the 564 patients was 9.7 ± 3.0 years. The gender and age did not differ significantly between the perforation and non-perforation groups. In the perforation group, nausea and vomiting were more frequent, and the duration of symptoms and median length of hospital stay were longer. The median WBC and neutrophil counts, neutrophil-to-lymphocyte ratio, ESR, and CRP concentration were significantly higher in the perforation group (Table 1).
Predictors of PA
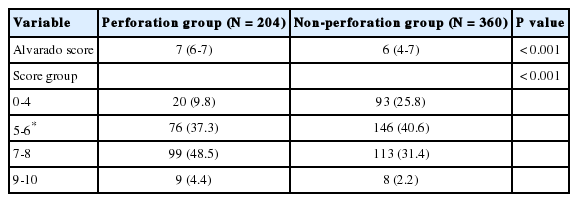
Fig. 1 depicts the AUCs of inflammatory markers and the Alvarado score, and among these variables, CRP concentration had the highest AUC. The AUC for CRP concentration was 0.72 (95% CI, 0.68-0.76; P < 0.001), with a cutoff of 25.7 mg/L, and AUC for WBC count was 0.71 (95% CI, 0.67-0.74; P < 0.001), with a cutoff of 13.5 × 109/L. The AUC of the Alvarado score was 0.63 (95% CI, 0.59-0.68; P < 0.001). The perforation group showed higher median Alvarado score, and had more patients having the Alvarado score ≥ 7 (Table 2).
The receiver operating characteristic curves of inflammatory markers to predict perforated appendicitis. CRP concentration had the highest AUC (0.72), followed by WBC count (0.71). AUC: area under the curve, CI: confidence interval, CRP: C-reactive protein, WBC: white blood cell, ESR: erythrocyte sedimentation rate, NLR: neutrophil to lymphocyte ratio.
Overall, WBC count showed the highest sensitivity and NPV. An Alvarado score ≥ 6 for predicting PA had a 76.0% sensitivity, 43.9% specificity, 43.4% PPV, and 76.3% NPV. An ESR > 15.0 mm/h had a 59.3% sensitivity, 70.9% specificity, 53.7% PPV, and 75.3% NPV, while a WBC count > 13.5× 109/L had a 79.9% sensitivity, 53.9% specificity, 49.5% PPV, and 82.6% NPV. CRP concentration > 25.7 mg/L had a 14.6% sensitivity, 95.7% specificity, 65.9% PPV, and 66.5% NPV.
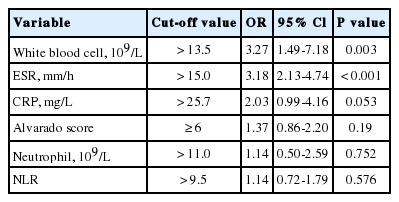
In the multivariable logistic regression analysis, WBC count > 13.5 × 109/L (OR, 3.27; 95% CI, 1.49-7.18; P = 0.003) and ESR > 15 mm/h (OR, 3.18; 95% CI, 2.13-4.74; P < 0.001) were independent predictors of PA in this study population, but CRP concentration was not (P = 0.053) (Table 3).
Discussion
This study found that a high WBC count (>13.5 × 109/L) and ESR (> 15.0 mm/h) are independent predictors of PA in the pediatric patients who visited the ED and subsequently had pathologically confirmed appendicitis. Early detection of PA in children is associated with the decrease in morbidity and mortality [17]. Our findings could help prediction of PA in the ED. However, the AUC for the Alvarado score ≥ 6 in PA alone yielded a poor discriminatory value.
Macklin et al [18]. reported a 76.3% sensitivity and 78.8% specificity with a cutoff Alvarado score of 7 for predicting appendicitis in pediatric patients. In another study that used computed tomography and the Alvarado score in predicting appendicitis, a score ≥ 6 had a 72.8% sensitivity and 61.6% specificity [19]. However, in our series, 20% of the patients with appendicitis had the scores of 0 to 4. Considering the inaccuracy of the Alvarado score in pediatric patients, predicting PA in pediatric patients using only this scoring system remains problematic.
If a patient has a high Alvarado score ≥ 6 points in the ED, inflammatory markers, such as WBC count and ESR, might help predict PA by increasing the sensitivity and NPV. Kafetzis et al [20]. showed that a WBC count > 10.0 × 109/L had a 87.5% sensitivity and 88% NPV for PA in pediatric patients. We obtained a comparable sensitivity and a NPV of WBC count. Another study showed that WBC count combined with CRP concentration had a 96% specificity for PA [13]. Few studies have evaluated the association between ESR and PA [12,16]. One study reported that pediatric patients with PA had a significantly higher ESR than those without PA, although the ESR was measured in a small portion of the patients with appendicitis [12]. Our study shows a relatively low ESR cutoff. In another study, ESR showed a poor correlation with the type of appendicitis [16]. The role of ESR in predicting PA might have been undervalued, and further prospective studies regarding its diagnostic value are needed.
CRP may not always be useful for predicting PA in pediatric patients. An elevated CRP concentration has been reported as a better predictor of PA than the WBC count in adult patients with appendicitis [19,21]. In pediatric patients, CRP has been reported to predict PA [11,22]. A prospective study found that pediatric patients with a CRP concentration > 30 mg/L or a procalcitonin level > 0.2 ng/mL had a greater predictor of PA [11]. However, our study shows lower cutoff of CRP concentration and no association between CRP and PA. This finding may be due to time-dependent changes of CRP concentration. CRP is more accurate after 24 to 48 hours from the symptom onset [23]. In this study, more than 50% of the pediatric patients visited the ED within 24 hours of symptom onset.
The limitations of this study are related to its relatively small study population and retrospective design. First, we included patients with appendicitis seen in the ED, implying the possible selection bias. However, this limitation does not seem critical given that the median age, proportion of boys and PA were comparable to previous studies [12,24]. Second, given the retrospective design, the Alvarado score may have been underestimated due to the lack of information.
In conclusion, a high WBC count (> 13.5 × 109/L) and ESR (> 15.0 mm/h) might be associated with PA in pediatric patients with appendicitis. Conversely, the Alvarado score and CRP concentration may be inadequate to predict PA.
Notes
Conflicts of interest
We declare that we have no conflict of interest relevant to this article.
Acknowledgements
We did not receive any financial support for this report.