코로나바이러스감염증-19 범유행 기간 보호장구 탈착 정책이 응급실 체류시간에 미치는 잠재적 영향
A potential impact of the donning and doffing policy on emergency department length of stay during the coronavirus disease 2019 pandemic
Article information
To the editors,
Coronavirus disease 2019 (COVID-19) pandemic is a worldwide challenging public health condition. Italy has been fighting against the pandemic. Although children seem to be relatively spared by the infection, the governmental rules for COVID-19 re-organization profoundly involved pediatric hospitals.
The third level Gaslini Institute is a main pediatric hospital in Italy, and provides regional, national, and extra-national pediatric care. During pre-pandemic period, the emergency department (ED) had 35,000-37,000 visits per year. Overall visits to Italian EDs decreased during the pandemic. This decrease may be explained by several reasons: patients’ and their parents’ fear of nosocomial infection, continuous warning messages from government authorities, and decrease in infection and injury due to the closure of schools and sports venues[1-4]. Gaslini institutional COVID-19 guidelines established that every patient asking for a non-scheduled visit to the hospital must pass through the ED, and is regarded as infected until proven otherwise. The first measures include a pre-triage interview, use of a dedicated path, and a detailed donning and doffing policy applied for each visit.
From the beginning of the crisis (March 10, 2020) to the time of this writing (December 31, 2020), the overall number of ED visits was about 15,000, which was fewer than that during the same period in 2019 (about 29,000). In the beginning and during the 2 waves of COVID-19 (March-April and September-November 2020), we initially intended to optimize the donning and doffing policy and to standardize operational procedures, while initially ignoring the potential impact of the policy on time intervals. As the days went by, an increase in ED length of stay (EDLOS) was noted in the process of implementing the donning and doffing policy. Vitally, we noted a 32%-56% increase in the calculated EDLOS during the pandemic (Fig. 1). Based on this figure, we can confirm that the overall number of patients whom emergency physicians can ideally care was 72 per day pre-COVID-19, and that it was reduced to less than 50 per day. The increase in EDLOS has not been affecting the ED flow simply because of the overall decrease in the visits. We assume that the seasonal increase of infectious and respiratory diseases may be accompanied by a low but inexorably gradual recovery of ED visits. It may not be possible to maintain the current institutional guidelines if we encounter usual pre-pandemic ED visits with the current number of medical personnel.
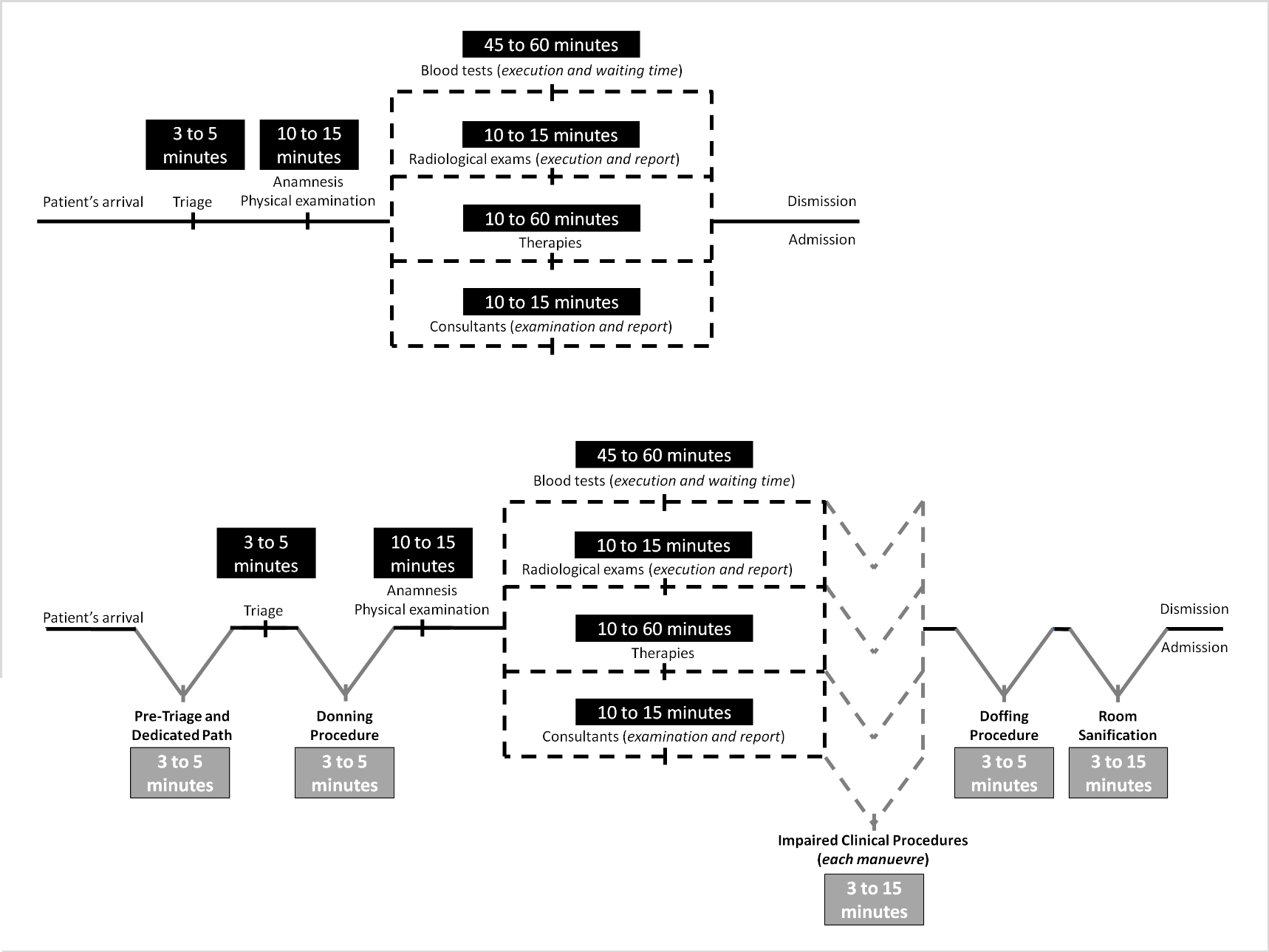
Calculated increased emergency department length of stay during March to December 2020 with a 32%-56% increase compared to that during March to December 2019. Eemergency department length of stay refers to a time interval from the patient’s arrival to discharge or transfer.
The authors believe that it was essential to promptly react to the pandemic. However, even more importantly, the government and local authorities should continuously evaluate the potential impact of the donning and doffing policy on EDLOS during the pandemic to prevent unexpected problems.
Notes
Conflicts of interest
No potential conflicts of interest relevant to this article were reported.
Acknowledgements
No funding source relevant to this article was reported.
