9세 환자에서 발생한 심장 기형을 동반하지 않은 심방세동
Atrial fibrillation without cardiac anomaly in a 9-year-old child
Article information
Trans Abstract
Atrial fibrillation (AF), the most common chronic arrhythmia in adults, is rarely reported in children. Moreover, most of the previously reported children with AF have comorbidities, such as structural heart diseases, rheumatic diseases, and thyroid diseases. This case report is about a healthy 9-year-old boy who was diagnosed with AF without cardiac anomaly. He visited the emergency department with chest pain and palpitation, lasting 2 hours. His electrocardiogram showed narrow-complex tachycardia, which led to the diagnosis of supraventricular tachycardia. The administration of adenosine revealed rapid irregular P waves. After electrical cardioversion, cardiac rhythm was converted to normal sinus rhythm. This case report suggests that when children with narrow-complex tachycardia visit the emergency department, the possibility of AF, in addition to supraventricular tachycardia, should be considered if the RR intervals are markedly irregular.
Introduction
Atrial fibrillation (AF), the most common arrhythmia in adults, is rare in children and infants. The typical clinical background for AF to occur in children includes congenital heart disease, cardiomyopathy, and Wolff-Parkinson-White syndrome [1]. AF may also be caused by hyperthyroidism or rheumatic disease. AF occurring in younger patients without underlying cardiovascular disease or comorbidities represents less than 5% of all types of AF [2].
Patients with AF usually experience palpitation, exercise intolerance, chest pain, and shortness of breath. Those with compromised ventricular function and particularly slow or fast ventricular response rate may experience weakness due to congestive heart failure in addition to palpitation [3]. Persistent or recurrent AF carries inherent risks and morbidities, such as stroke, heart failure, and death. Hence, AF should be diagnosed quickly and accurately in the emergency department (ED). Moreover, as AF is easily overlooked in pediatric practice because of the low incidence in children, a careful diagnosis should be made.
Recently, we treated a boy who presented with chest pain and palpitation. Eventually, he was diagnosed with AF without cardiac anomaly.
Case
A healthy 9-year-old boy visited the ED at Hallym University Sacred Heart Hospital with continuous chest pain and palpitation, lasting 2 hours after bumping his chest to his friend. He was otherwise healthy except 1 episode of supraventricular tachycardia (SVT) presenting with palpitation, which occurred 7 months before this visit. No family history was found on any cardiovascular disease. He was not taking any medication, including alternative medicines, at the time of the visit.
Upon arrival at the ED, his height was 128.4 cm (5th to 10th percentile), weight 31 kg (25th to 50th percentile), and body mass index 18.8 kg/m2 (50th to 75th percentile). The initial vital signs were as follows: blood pressure, 110/70 mmHg; heart rate, 180 beats per minute; respiratory rate, 25 breaths per minute. His breathing sound was normal, the heart beat was fast and irregular without cardiac murmur. Physical examination was otherwise unremarkable. According to the chest radiograph, the cardiothoracic ratio was 0.53. Findings of initial electrocardiogram (ECG) are shown in Fig. 1A.
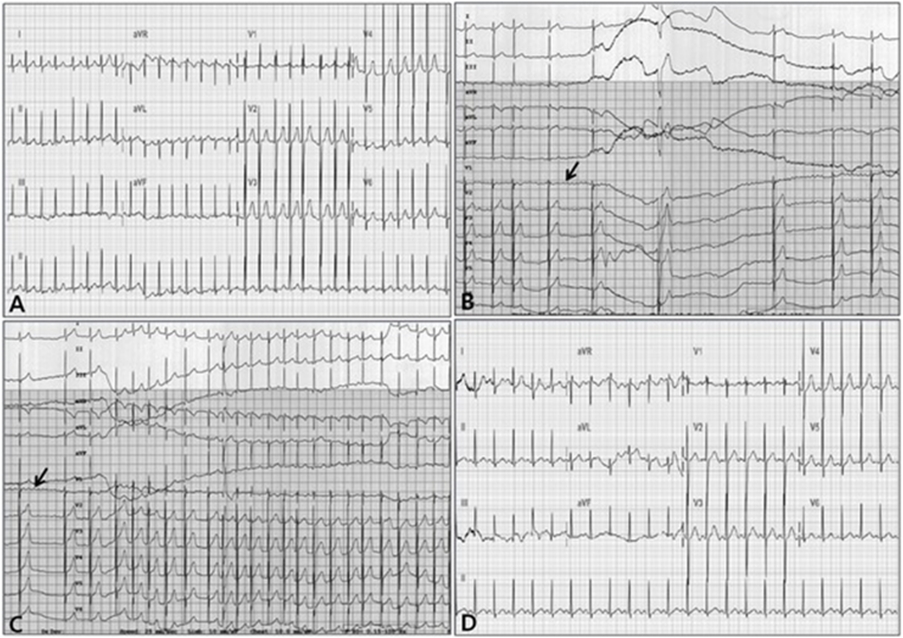
Initial electrocardiogram showing irregular RR intervals and absence of P waves. The ventricular rate was 180 beats per minute, QRS interval was approximately 60 msec, and QRS axis was within the normal range (A). Irregular P waves (arrows) were monitored immediately after administration of adenosine (B, C). Electrocardiogram after an electrical cardioversion shows sinus conversion (D).
Considering the past medical history, we deemed his condition as a recurrent episode of SVT. At first, we administered adenosine at a dose of 0.1 mg/kg. Since no sinus conversion occurred, we assumed that insufficient bolus had reached the systemic circulation due to short half-life of adenosine. No rhythm change was observed even after we injected additional 0.1 mg/kg. In total, 0.2 mg/kg of adenosine was administered. As the heart rate decreased immediately after the administration of adenosine, rapid irregular P waves resembling a sawtooth were observed, enabling us to diagnose it as AF (Fig. 1B, C). Since the boy visited the ED 2 hours after the symptoms appeared, no anticoagulant was administered before electrical cardioversion. Subsequently, after the cardioversion with 30 J (1 J/kg), sinus conversion occurred, then chest pain and palpitation were relieved (Fig. 1D). ECG after the sinus conversion showed the ventricular rate of 144 beats per minute, PR interval of 124 msec, corrected QT interval of 446 msec, and QRS axis of 67°, which were all within the normal ranges. Initial laboratory evaluation, including complete blood cell count, serum electrolyte, C-reactive protein, cardiac enzyme, and thyroid function test, showed no abnormalities. No remarkable structural and functional abnormalities were observed in the echocardiography.
The boy was hemodynamically stable after the electrical cardioversion, and was transferred to another hospital at his parents’ request. At the hospital, 24-hour Holter monitoring and exercise ECG showed no abnormalities. An electrophysiology study was not performed because the patient was not old enough to undergo the test and his symptoms had resolved. He did not receive any prescription for AF.
After 5 months, he returned to the ED with narrow-complex tachycardia. At that time, he was diagnosed with SVT (Fig. 2A), and sinus conversion occurred after the administration of adenosine (Fig. 2B). He has been taking atenolol for 7 months without recurrence of both AF and SVT.
Discussion
AF is considered to arise from multiple small migratory reentry circuits occurring predominantly in the left atrium. Although AF is common in elderly patients, this entity is rare in children. This low incidence is possibly due to the atrial size that is inadequate to support multiple circuits [3]. Among children, AF occurs predominantly in association with underlying heart disease, most often following surgery for congenital heart disease [4]. Conversely, among infants, AF usually occurs in the structurally normal hearts, and is instead frequently associated with the existence of an accessory pathway. Older children and adolescents with Wolff-Parkinson-White syndrome are also susceptible to AF, and this susceptibility poses a risk for ventricular fibrillation due to the pre-excited AF.
The etiology of AF in children with structurally normal heart is secondary to alcohol or drug abuse, stimulant medications, caffeine, changes in the autonomic tone, and exercise [5,6]. In our case, AF occurred in a healthy boy without cardiac anomaly (i.e., lone AF).
AF can be diagnosed by ECG, which shows the marked irregularity in the RR intervals and the inconsistent pattern of atrial depolarization. The diagnosis of AF in children is not difficult in most cases. However, like our case, misdiagnosing AF as SVT is possible due to pediatricians’ limited experience in AF with rapid ventricular rates. In this situation, intravenous adenosine and transesophageal or transthoracic electrode recording can be used to assist in the diagnosis [7].
Our patient had undergone 2 episodes of SVT, one before and one after the episode of AF. Two studies have reported the association between SVT and AF. One study demonstrated that 39% of children and adolescents with lone AF had an additional form of SVT discovered during a formal electrophysiology study [8]. The other study reported approximately 10% of adult patients with lone AF had inducible SVT in an electrophysiology study [9]. Conversely, SVT is known to degenerate into AF via 2 mechanisms. AF may be induced by fast atrial activation or by adenosine injection [10,11]. Thus, the children who had an event of SVT or AF should be informed that both SVT and AF may occur afterwards. Antiarrhythmic drugs or catheter ablation should be considered in children with recurrent symptomatic AF [12].
In conclusion, when children with narrow-complex tachycardia visit the ED, the possibility of AF should be considered in addition to SVT, given the marked irregularity in RR intervals.
Notes
Conflicts of interest
No potential conflicts of interest relevant to this article were reported.
Acknowledgements
No funding source relevant to this article was reported.

